The ABCs of Picking a Medigap Policy
For those enrolling in traditional Medicare, buying a supplemental insurance policy covers the substantial gaps left by deductibles and co-payments.

Profit and prosper with the best of Kiplinger's advice on investing, taxes, retirement, personal finance and much more. Delivered daily. Enter your email in the box and click Sign Me Up.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered daily
Kiplinger Today
Profit and prosper with the best of Kiplinger's advice on investing, taxes, retirement, personal finance and much more delivered daily. Smart money moves start here.

Sent five days a week
Kiplinger A Step Ahead
Get practical help to make better financial decisions in your everyday life, from spending to savings on top deals.

Delivered daily
Kiplinger Closing Bell
Get today's biggest financial and investing headlines delivered to your inbox every day the U.S. stock market is open.

Sent twice a week
Kiplinger Adviser Intel
Financial pros across the country share best practices and fresh tactics to preserve and grow your wealth.

Delivered weekly
Kiplinger Tax Tips
Trim your federal and state tax bills with practical tax-planning and tax-cutting strategies.

Sent twice a week
Kiplinger Retirement Tips
Your twice-a-week guide to planning and enjoying a financially secure and richly rewarding retirement

Sent bimonthly.
Kiplinger Adviser Angle
Insights for advisers, wealth managers and other financial professionals.

Sent twice a week
Kiplinger Investing Weekly
Your twice-a-week roundup of promising stocks, funds, companies and industries you should consider, ones you should avoid, and why.

Sent weekly for six weeks
Kiplinger Invest for Retirement
Your step-by-step six-part series on how to invest for retirement, from devising a successful strategy to exactly which investments to choose.
People who are enrolling in traditional Medicare should buy a supplemental insurance policy to cover the substantial gaps left by deductibles and co-payments, according to consumer advocates. But choosing a private Medigap plan can be daunting.
That's what Joyce Katen discovered when she turned 65 in May. "I got so confused," says Katen, a clothing manufacturing consultant in New York City. She turned to the Medicare Rights Center (www.medicarerights.org), a consumer group that helped her choose an insurance policy among numerous offerings.
Like others approaching 65, Katen first needed to decide how she would protect herself against Medicare's large coverage gaps. Most beneficiaries have two options. They can go with a private Advantage plan, which covers all Medicare benefits, provides drug coverage and limits out-of-pocket costs. Or they can opt for traditional Medicare and buy a separate Medigap policy as well as a Part D prescription-drug plan.
From just $107.88 $24.99 for Kiplinger Personal Finance
Become a smarter, better informed investor. Subscribe from just $107.88 $24.99, plus get up to 4 Special Issues

Sign up for Kiplinger’s Free Newsletters
Profit and prosper with the best of expert advice on investing, taxes, retirement, personal finance and more - straight to your e-mail.
Profit and prosper with the best of expert advice - straight to your e-mail.
For Katen, that decision was easy. Advantage plans restrict your selection of providers, and Katen says she wants to be able to use any doctor she chooses, as traditional Medicare allows.
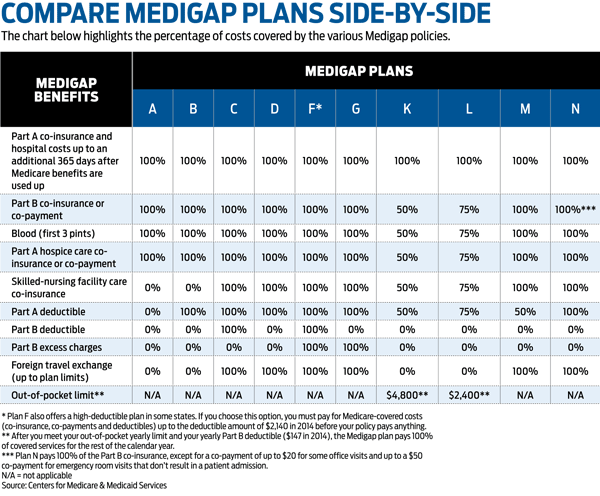
Then came the hard part for Katen: choosing a supplemental insurance policy. Medigap policies are sold by private insurers in ten standardized benefit designs, named A through N. With some exceptions, coverage and price generally increase as you move up the alphabet.
Plans C and F are held by a majority of the nine million Medigap beneficiaries. Both plans pay the deductible for Part A, which covers hospital costs, and for Part B, which covers outpatient costs. The deductible for Part A will be $1,260 for each benefit period in 2015, and the annual Part B deductible will be $147. (Plans E, H, I and J are no longer sold, but if you hold one, you can continue to keep it in most cases.)
To figure out which policy is best for you, consider your "health status, family medical history and risk tolerance," says Casey Schwarz, policy and client services counsel for the Medicare Rights Center. Healthier beneficiaries who rarely need medical care may be best suited for high-deductible plans.
Plans K and L are high-deductible policies that have lower premiums but impose higher out-of-pocket costs. Plan F also offers a high-deductible version.
But new beneficiaries should not choose a plan based solely on their health today. As long as you buy a Medigap policy within six months of enrolling in Part B, an insurer cannot reject you or charge you more because of medical issues. If you become ill and want to switch to a plan with better coverage, an insurer can boost the cost or turn you down.
Katen decided to go with the fully loaded Plan F. Katen, who is healthy, would rather pay more for comprehensive coverage and not worry about footing the bill if she gets sick. "I can't imagine not having the coverage," she says. She pays UnitedHealthcare, which sells policies under the AARP name, a monthly premium of $261, in addition to the monthly $104.90 Part B premium she pays to Medicare.
Find a Plan That Fits Your Needs
Depending on the plans offered in your area, Plan N could be a middle ground for many healthy beneficiaries. "Plan N provides very good coverage and is more affordable than Plan F," says Ross Blair, senior vice-president of eHealthMedicare.com, a division of online broker eHealth Inc. Plan N provides much of the same coverage as Plan F, but it doesn't cover the $147 Part B deductible. It also charges a $20 co-payment for doctor visits and a $50 co-payment for emergency room visits that don't result in hospital admissions.
In New York City, UnitedHealthcare offers a Part N plan for $178 a month, compared with Katen's $261 premium for Plan F. Katen could still come out ahead with Plan N if she had two emergency room visits and 40 visits to the doctor.
Once you choose your plan category, it usually makes sense to go with the cheapest plan. Under federal law, all plans offered under the same letter must offer the same benefits. Prices for the same policy can vary widely. For example, annual Plan F premiums range from $1,752 to $3,768 in Rockville, Md., and from $2,472 to $6,552 in Miami.
Besides checking the initial premium, ask the insurer which of the three pricing methods it uses for the plan you are considering. Attained-age pricing bases the premium on your age when you buy the policy, with rates rising as you grow older. Premiums can also increase because of inflation.
With issue-age pricing, the premium is based on the age at which you buy the policy (the younger you buy, the less expensive), and it will not change as you age, except for inflation. Community-rated policies charge the same price to everyone regardless of age, and your annual premium can only increase for inflation. "We would encourage going with a community-rated plan, with an issue-age plan being the next best thing," Blair says. He compares attained-age policies to variable-rate mortgages, which start off at a low price but can escalate considerably.
To understand how your costs may change over time, ask for a three- to five-year rate history for each policy you are considering. Also ask for quotes as if you were age 70, 75 and 80. Some insurers will offer discounts -- for nonsmokers, for women and for those who hold several policies with the company, such as homeowners and auto insurance.
While companies in most states can conduct medical underwriting if you apply for a plan after the initial six months are over, there are some exceptions. You can buy Medigap coverage without underwriting if you're in a Medicare Advantage plan and you move out of its service area, or if your insurer stops selling the Medigap plan you currently have. Another exception is if your retiree health coverage from a former employer ends. And some states, such as New York, prohibit underwriting after the six-month period.
To compare policies in your area, visit www.medicare.gov/find-a-plan/questions/medigap-home.aspx. To get additional help, get in touch with your local State Health Insurance Assistance Program at www.shiptalk.org. You'll find rules in your state by visiting the Web site of the National Association of Insurance Commissioners (www.naic.org). Note that Massachusetts, Minnesota and Wisconsin have their own standardized benefits.
Profit and prosper with the best of Kiplinger's advice on investing, taxes, retirement, personal finance and much more. Delivered daily. Enter your email in the box and click Sign Me Up.
-
 Nasdaq Leads a Rocky Risk-On Rally: Stock Market Today
Nasdaq Leads a Rocky Risk-On Rally: Stock Market TodayAnother worrying bout of late-session weakness couldn't take down the main equity indexes on Wednesday.
-
 Quiz: Do You Know How to Avoid the "Medigap Trap?"
Quiz: Do You Know How to Avoid the "Medigap Trap?"Quiz Test your basic knowledge of the "Medigap Trap" in our quick quiz.
-
 5 Top Tax-Efficient Mutual Funds for Smarter Investing
5 Top Tax-Efficient Mutual Funds for Smarter InvestingMutual funds are many things, but "tax-friendly" usually isn't one of them. These are the exceptions.
-
 9 Types of Insurance You Probably Don't Need
9 Types of Insurance You Probably Don't NeedFinancial Planning If you're paying for these types of insurance, you might be wasting your money. Here's what you need to know.
-
 Amazon Resale: Where Amazon Prime Returns Become Your Online Bargains
Amazon Resale: Where Amazon Prime Returns Become Your Online BargainsFeature Amazon Resale products may have some imperfections, but that often leads to wildly discounted prices.
-
 457 Plan Contribution Limits for 2026
457 Plan Contribution Limits for 2026Retirement plans There are higher 457 plan contribution limits in 2026. That's good news for state and local government employees.
-
 Medicare Basics: 12 Things You Need to Know
Medicare Basics: 12 Things You Need to KnowMedicare There's Medicare Part A, Part B, Part D, Medigap plans, Medicare Advantage plans and so on. We sort out the confusion about signing up for Medicare — and much more.
-
 The Seven Worst Assets to Leave Your Kids or Grandkids
The Seven Worst Assets to Leave Your Kids or Grandkidsinheritance Leaving these assets to your loved ones may be more trouble than it’s worth. Here's how to avoid adding to their grief after you're gone.
-
 SEP IRA Contribution Limits for 2026
SEP IRA Contribution Limits for 2026SEP IRA A good option for small business owners, SEP IRAs allow individual annual contributions of as much as $70,000 in 2025, and up to $72,000 in 2026.
-
 Roth IRA Contribution Limits for 2026
Roth IRA Contribution Limits for 2026Roth IRAs Roth IRAs allow you to save for retirement with after-tax dollars while you're working, and then withdraw those contributions and earnings tax-free when you retire. Here's a look at 2026 limits and income-based phaseouts.
-
 SIMPLE IRA Contribution Limits for 2026
SIMPLE IRA Contribution Limits for 2026simple IRA For 2026, the SIMPLE IRA contribution limit rises to $17,000, with a $4,000 catch-up for those 50 and over, totaling $21,000.